As most people with MND are cared for at home, if an acute incident occurs, they will need to access crisis intervention services.
Our information for professionals in acute, urgent and emergency care is designed to give succinct guidance on actions to take and things to consider when treating someone with the condition.
Looking for all our resources for a specific profession or topic, for you and the people you support?
Use our Professional Information Finder
Key points when you have a patient with MND
Check for the following documents in the person’s records Emergency healthcare plan
- Advance care plan – this includes preferences for care, including place of care and end of life decisions
- Advance Decision to Refuse Treatment (ADRT) – if the person has created and signed an ADRT, this must be considered
- Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) – the person may have specified a DNACPR, which must be considered
- MND Alert Card or Understanding My Needs – these include key contacts and information about their care team and the specialist help they may need.
A person with MND may have a high NEWS (National Early Warning) score
However, this could be normal for that person. They will have a normal increased respiratory rate and also a lower Sp02 that needs to be taken into account. Establish if this has changed.
Communication
Find out how the person communicates. Speaking can be very difficult, or impossible, for people with MND. They may normally use a communication aid and should be helped to use this, if appropriate.
Oxygen caution
Patients with respiratory failure due to chronic neuromuscular weakness (seen in MND) will rapidly retain carbon dioxide. Supplementary oxygen therapy can have a serious detrimental effect in people with MND, reducing respiratory drive and worsening their condition.
Oxygen therapy (unless as a palliative measure, which may be appropriate) should be used with great caution in patients with MND-related respiratory problems and monitored by arterial blood gas analysis.
Seek guidance from the specialist palliative care team or a respiratory consultant with links to neurology.
The patient may not be able to lie flat, even for x-rays/scans
This is due to decline of respiratory function in MND.
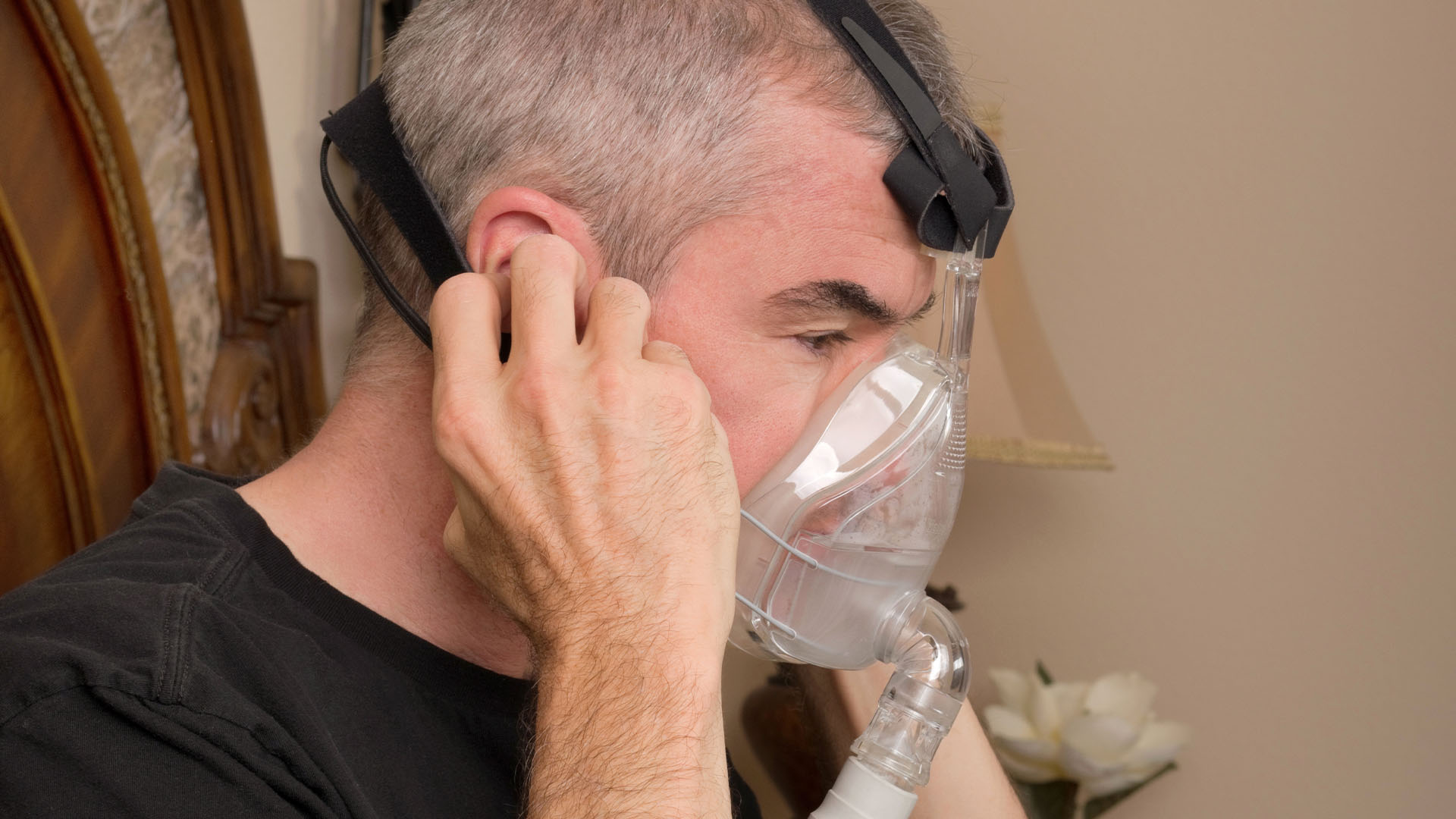
Does the patient use a non-invasive ventilator?
If airways are clear, reapply non-invasive ventilation (NIV) to treat breathlessness. Visit our pages on respiratory symptoms in MND for further information.
Does the patient appear to have cognitive change or dementia?
About 50% of people with MND are affected by cognitive and/or behavioural change, increasing to 80% in the final stages of the disease.
Some people experience very mild changes which are barely noticeable, whereas for others the changes can be more pronounced. Around 15% of people with MND will develop frontotemporal dementia (FTD).
In some cases, cognitive change may impact on decision making.
For more detailed information on cognitive change and dementia in MND, visit www.mndassociation.org/cognition
Is the patient pyrexial and taking riluzole?
Check full blood count (FBC) for signs of neutropenia and liver function tests (LFTs) for sign of disturbance, especially alanine transaminase (ALT).
Locate the next of kin
If next of kin is not present, every attempt should be made to contact them in case crucial decisions need to be made. Once located, take account of their insight into the person’s condition and care needs.
Does the patient have an enteral feeding tube?
This will affect decisions around administration of medication (including route and type) and fluids.
Consider the administration route of any drug you choose to prescribe
Especially if the patient has swallowing difficulties and no enteral feeding tube.
Contact your local MND care centre/network for specialist advice and support
Where available, contact the specialist team in your hospital or local area. See details of MND Care Centres and Networks.
Page last updated: July 2023
Next review: July 2025