As MND is a progressive condition, a person’s care needs will greatly increase over time and they will need more support from others.
This section has been designed to give you information and practical tips on the care of someone with MND. It will help you find out more about MND, whether you care for someone with the condition now or in the future.
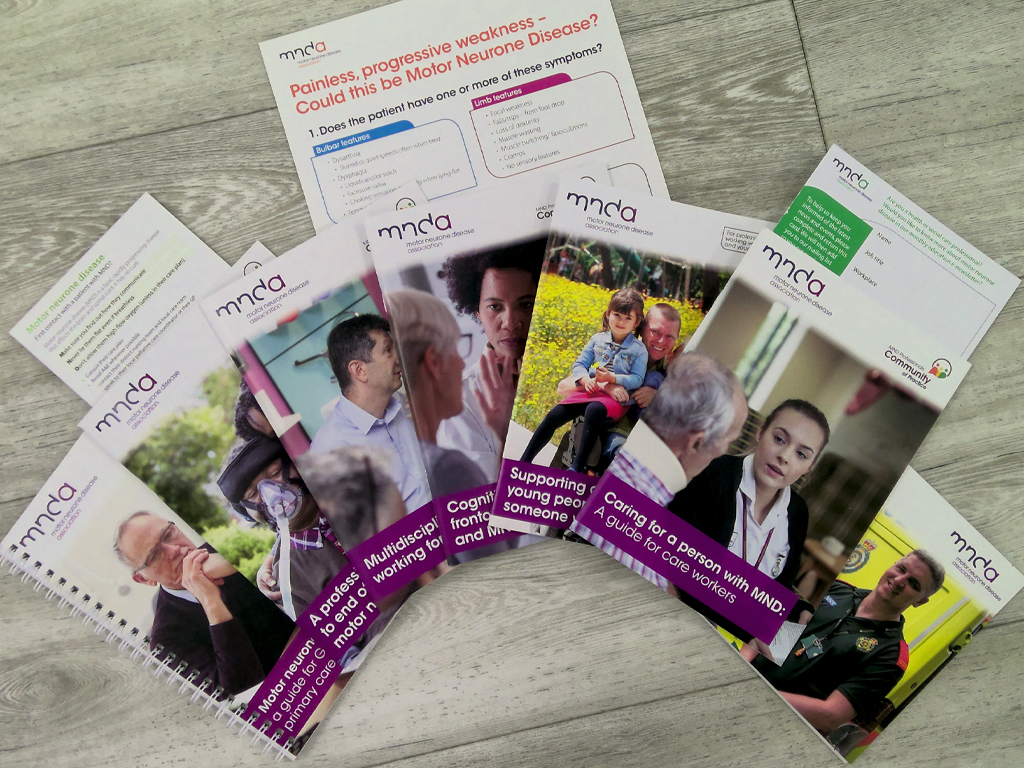
Looking for all our resources for a specific profession or topic, for you and the people you support?
Use our Professional Information Finder
The role of the care worker
As a care worker, you play a key role in helping to maintain quality of life for a person with MND.
You may be in more frequent contact with the person than other professionals involved in their care, so you will have a good overview of how they are day to day and will become aware of changes in their condition, or any extra needs they have.
With MND, it can be difficult to predict what might happen next and what support might be needed. If you notice any early signs of change and alert the right people, this may help to get support in place sooner.
If you are able to give detailed, objective feedback on the person’s condition and any changes, this can be very useful for other professionals who are providing care.
There may be a range of professionals involved in the care of a person with MND. This is often called the multidisciplinary team. As a professional care worker, you are a key part of the team.
Referral to other services and sources of support
When you first start caring for someone, find out who you would need to contact if certain issues or queries come up.
If you think the person with MND would benefit from extra support:
- encourage the person to raise this with their GP or specialist team
- report the issue to your manager or supervisor who should contact the person’s GP or specialist team
- speak to the person’s GP or MND team if you have direct contact.
Working with the person’s unpaid carers
The person with MND, and any unpaid carers they have, should also be seen as part of the multidisciplinary team. They will have expert knowledge of the condition and its effects. If the person has family around them, they will often be part of the care team.
Good communication with the person’s unpaid carer(s) is vital if you are providing care in addition to the care they provide, especially if you are working within their home. While a professional carer may be involved to provide respite breaks for family carers, family carers may also step in to allow professional carers to have breaks from their caring duties. During the handover of responsibilities, they will need to be made aware of any developments or changes in procedures. Alongside the person with MND, the family will also be very influential in executive decision-making, so precise communication with family members is very important.
Working with ambulance staff or paramedics
If the person with MND needs to be taken to hospital in an emergency, don’t be afraid to offer information that may help the ambulance staff or paramedics. Ambulance staff may not know very much about MND and might not be aware, for example, that they should not:
- lie the person flat
- automatically give the person oxygen, unless it is under guidance of an MND specialist.
Training to help you care for a person with MND
To care effectively for a person with MND, you will need training in:
- MND – including how it progresses and important markers to look out for
- good communication skills – a care worker should know how to communicate with, and understand the needs of, a person who may have lost or has difficulty with their speech
- moving and handling
- safeguarding
- dignity in care provision
- cognitive change and dementia.
Further training should also be available if needed, in:
- assisting with medication
- helping a person who has a feeding tube
- using an assisted ventilation machine and other equipment.
- The training given by care agencies will usually cover basic skills, but often will not cover specific information about the care of people with MND or how to use specialist pieces of equipment. There may be many different pieces of equipment you need to use when caring for a person with MND.
Training in specific areas of care should be provided by relevant members of the person’s health and social care team. See next heading Care worker module to find out more about our free online course for care workers.
Care worker module
Our free online module for care workers introduces MND, its symptoms, and the support a care worker can give to a person with MND.
This introductory level module is split into seven units:
- Introduction to MND
- Eating and Swallowing
- Breathing
- Moving
- Thinking
- Communicating
- End of life
Care planning
MND affects every individual differently. People with MND should have a full assessment of their care needs, which includes their preferences, likes and dislikes.
A detailed, personalised care plan and statements of preferences should result from a discussion with the person with MND about the whole picture of needs they have: health, personal, family, social, economic, educational, mental health, and ethnic and cultural background. It should draw on information from the person with MND and relevant health and social care professionals involved in their care.
A key member of the person’s health and social care team will be responsible for having this conversation and designing the plan with the person with MND. The plan will involve a number of organisations and professionals who will be directed by a key worker. This may be a relative.
Because of the progressive nature of MND, a care plan for a person with the condition should be regularly reviewed in order to respond to ongoing changes in needs. This review should be carried out by a professional who can support the person with MND and those around them through the process. As a care worker, you should follow this plan and report back to your supervisor when needs are changing and a review is required.
Caring for a person with MND
Personal care
- For people with MND, washing, dressing and toileting can take a long time.
- People who need help to wash, dress or use the toilet often experience feelings of indignity. This can be even more of an issue if rapid progression of MND has brought sudden change.
- Privacy in these and all areas of personal care is vital.
- Personal space should be respected.
- If people are able to carry out tasks for themselves and do not fatigue easily, this can improve morale and dignity.
- The support a person receives from their professional team can help them to maintain dignity.
- An occupational therapist can recommend strategies and equipment to help with personal care.
- Some people may choose to take a more dependent role, despite being able to do things for themselves.
Movement and handling
The loss of muscle bulk and strength can make joints stiff and painful. Care is needed when lifting, handling and positioning to avoid causing any further pain or the dislocation of weak joints. You should receive training on how to move the person without causing distress.
A physiotherapist and/or occupational therapist should carry out a full assessment to identify the movement and handling needs of the person with MND and their carers. They should talk to you about:
- safe techniques for handling people with MND who have fallen
- how the limbs, head and neck should be supported during transfers
- equipment that may help, such as sliding sheets, hoists, profiling beds, mattress elevators, riser-recliner chairs and turning tables.
Positioning to help with breathing problems
If a person has respiratory problems, they will feel breathless when lying flat and this may be uncomfortable and scary. It is important to find positions that make it easier for the person with MND to breathe. The ideal position is usually upright or slightly reclined, with the arms, back, head and neck supported.
A semi-reclined position may be achieved by using a riser-recliner chair with arm supports, or a wheelchair with tilt-in-space. This position allows the diaphragm to move more freely and efficiently, it will help the person to maintain a good head position and will make it easier to swallow.
In bed, a semi-reclined position is likely to be more comfortable. A raised head, perhaps with more pillows, a pillow lifter or a profiling bed, may reduce night-time problems.
If breathing is laboured
- A physiotherapist can teach or give advice on techniques to help with breathing, including posture and positioning, and clearing secretions.
- An occupational therapist can give advice on posture and positioning, as well as helping to identify equipment to help with positioning.
- Some people with MND find it helpful to have an electric fan blow air into their face, as it provides some psychological relief when breathless.
Pressure care
- If a person with MND is using a mask for non-invasive ventilation, they may get pressure sores on the bridge of their nose. Their face shape may change as MND progresses and muscles waste, meaning the mask doesn’t fit as well as it once did. A respiratory physiotherapist can recommend alternative mask designs, or address any concern about the mask not having a good enough seal.
- Good skin and pressure care is vital to prevent sores. A person with MND may be aware of when they need to be turned or moved, but may need help to adjust their position.
- Consider appropriate equipment for skin sensitivity relief, such as a bed cradle to relieve the weight of bed clothes, lightweight bed clothing, a pressure-relieving mattress and cushions. Barrier creams may be applied to the skin to prevent pressure sores.
Clothing and temperature control
- Loose-fitting layers can help to trap heat, and it is easier to remove layers when hot.
- Different types of materials can help with temperature control – cotton and cotton-rich fabrics are usually best.
- Use warm socks for cold feet and warm up clothes before dressing.
Night time: disturbed sleep
People with MND may experience problems with sleep resulting from reduced mobility, muscle cramps, swallowing problems and anxiety. People may be afraid to sleep if they are aware they are not breathing fully and fear they will not wake. They may feel they haven’t slept well, have headaches, feel ‘hungover’ and may fall asleep during the day. It may be difficult to rouse the person from sleep and they may seem confused on waking.
These may be the first signs of problems with the respiratory system. They should be reported to the person’s healthcare team, who can refer the person for respiratory assessment. One of the first steps may include use of a profiling bed, which allows the person to sleep with their head and chest raised up, making breathing easier.
Bed comfort
Although a profiling bed may be recommended, it’s important to understand that a person living with MND may not wish to change their bed for many reasons: for example, if they share it with their partner or they find their bed comfortable. Any discussions about changing beds must be handled with sensitivity.
Eating and drinking
A dietitian should be involved in monitoring the weight and nutritional intake of the person with MND as the condition progresses. They can also give advice on the types of food to include and those to avoid while the person is still eating by mouth. If the person with MND has problems with swallowing, the dietitian will work with a speech and language therapist to introduce a diet where the person can get the most nutrition from what they eat and drink.
At mealtimes, an upright position can help to reduce the risk of aspiration. It might help to use the ‘chin-tuck’ or ‘chin-down’ posture, which involves tucking the chin to the chest when swallowing. This can prevent food going down into the airway. A speech and language therapist can teach the person with MND this technique.
An occupational therapist can give advice on equipment that may help at mealtimes.
These tips may be useful day to day:
- Serve several small meals rather than one large one: this can be less tiring for the person eating.
- Follow any advice given by the speech and language therapist about easy-to-swallow meals and food consistency. This may include using thickeners in fluids.
- Use garnishes and attractive colours to make food more appetising, and make sure the person eating can see and smell the food. This is especially important if food is mashed or puréed.
- Find out whether the person has preferences for particular comfort foods, such as puddings. Introduce small portions of these foods to create interest in eating and to promote wellbeing.
- Allow plenty of time for the meal.
- Keep food warm or reheat if necessary. A keep-warm plate may help.
- Let the person concentrate on what they’re doing – allow the person to swallow before asking questions.
- Leave a gap between courses if eating is slow and tiring.
- The person’s swallowing reflex may be stimulated by sipping a hot or cold drink before eating and between mouthfuls.
- A relaxed, quiet environment may help people to feel less anxious.
- The person with MND may feel unable to eat with other people because of swallowing problems. They may join others and take a few spoonfuls, while eating most of their meal before or afterwards.
Page last updated: July 2023
Next review: July 2025