This information is for health and social care professionals.
Swallowing problems affect at least two-thirds of all people with MND during the course of their illness.
When a patient presents with this symptom, deterioration is inevitable and referral to appropriate professionals should be made without delay.
See our information sheets for more detailed information:
Download our dysphagia information sheet
Download our saliva information sheet
View our bulbar weakness training video
View our dysphagia information for people with or affected by MND
Looking for all our resources for a specific profession or topic, for you and the people you support?
Use our Professional Information Finder
Dysphagia
Introduction
Dysphagia is a disruption of the normal eating and swallowing process. It affects many people during the course of MND.
People with MND may have swallowing problems caused by weak muscles in the bulbar region (face, mouth, tongue and throat). Those whose first symptoms affect this region (bulbar-onset) usually experience dysphagia at an earlier stage than those with other types of MND.
Swallowing problems in MND are caused by spasticity, largely resulting in weakness of the:
- tongue
- lips
- facial muscles
- pharynx and larynx.
Effects of dysphagia
Problems swallowing liquids results in coughing when drinking. This may be the first sign of early dysphagia.
Other signs include:
- loss of ability to form lip seal, chew food with the tongue and/or form a bolus
- poor or absent swallow reflex
- food not moving to the back of the mouth or disappearing down the throat due to a poor or absent swallow reflex, or an uncoordinated swallow caused by weak pharyngeal muscles
- muscle spasm
- more time needed for chewing, several swallows needed for each mouthful of food and becoming tired on eating and drinking
- a wet or muffled sounding voice after eating.
This can result in:
- sialorrhoea (drooling due to poor saliva control rather than excess production)
- dehydration and weight loss from not eating enough
- aspiration and recurrent chest infection
- problems swallowing medication
- tiredness and loss of strength and wellbeing
- lengthy mealtimes, leading to food going cold
- constipation.
There may be a social impact, too: the person with MND may feel unable to eat with other people due to dysphagia. They may join others and take a few spoonfuls, while eating most of their meal before or afterwards.
There may be times when a person with dysphagia will have episodes of coughing, sensations of choking or actual choking. Even though a choking episode is very distressing for them and their carer at the time, they can be reassured that it is virtually never a direct cause of death.
Role of professionals
As this symptom will get worse, it is crucial that referrals are made to the appropriate professionals as soon as a problem is identified. Referrals should be made by whichever professional first notices a problem.
Specialists at MND care centres or networks, or through multidisciplinary teams, can advise on dysphagia management and refer to appropriate services. The specialist respiratory team can determine whether the person with MND has respiratory involvement and risk of aspiration and/or choking, and can help the person with MND determine the course of action.
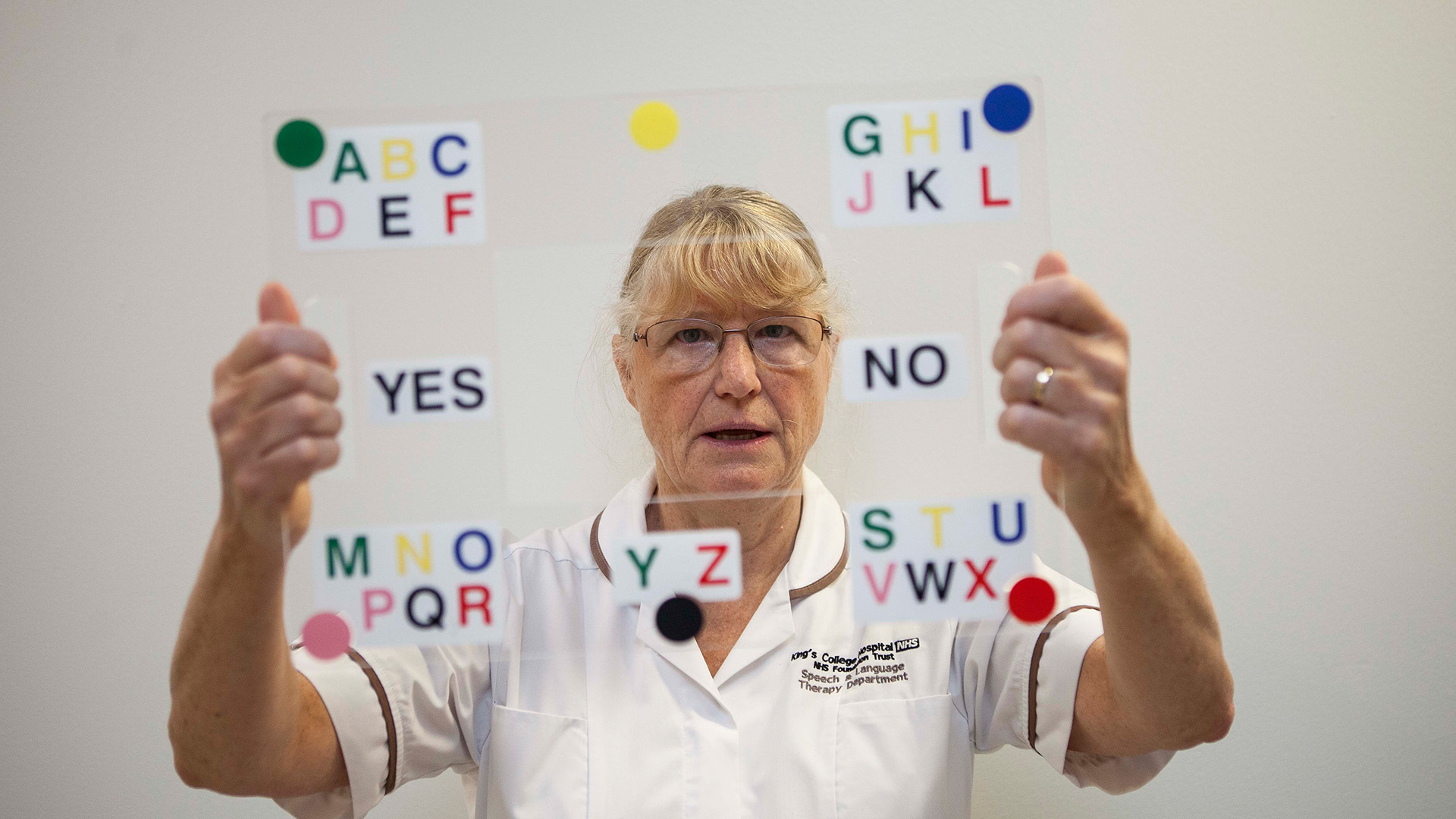
Referral to a speech and language therapist (SLT) should be a priority. They can assess the ability to eat and swallow and will put together a plan of action, which may include teaching swallowing techniques and altering the consistency of diet, for example by introducing a puréed diet. Often the SLT will indicate whether the person needs to see a dietitian and these two professionals will work closely together. Weak bulbar muscles will also affect communication. The SLT can assess speech problems and whether any aids or equipment might be needed to help the person with MND to communicate.
A dietitian can assess diet, nutritional and fluid intake and weight. Weight loss is often related to dysphagia, but it can also be affected by a person with MND not having the strength to feed themselves because of extreme fatigue or weakness in their upper limbs. Low mood or changes in bowel habit are other possible causes. A dietitian can suggest ways to optimise the person’s diet and nutritional intake. The person may be referred for an assessment for enteral feeding to determine whether alternative ways of feeding are needed.
A physiotherapist can advise on head supports and positioning and teach simple cough assist techniques to help with secretion management.
An occupational therapist may advise on head supports, seating and positioning, food and drink preparation, and may recommend strategies and equipment to help with eating and drinking, such as adapted cutlery.
Nutrition and enteral feeding
Weight loss and malnutrition
In people living with MND, unintentional weight loss and risk of malnutrition can result from:
- dysphagia
- depression
- cognitive impairment
- hypermetabolism
- anxiety
- respiratory insufficiency
- constipation and fatigue
- physical difficulties buying, preparing and eating foods.
Functional consequences of weight loss/malnutrition include:
- increased muscle wasting due to muscle catabolism
- increased respiratory muscle weakness
- decreased physical strength and mobility
- impaired immune function, which can increase susceptibility to opportunistic infections
- decreased tissue viability
- increased discomfort sitting or lying due to weight loss and loss of tissue ‘padding’ over bony protuberances
- decreased morale and quality of life.
Involvement of a speech and language therapist and a dietitian is essential at an early stage to assess, monitor and review the individual’s nutritional intake and to provide practical oral and non-oral dietary advice to enable nutritional needs to be met.
Advice may include:
- fortification to improve food quality
- recipe ideas to increase variety
- practical solutions to ease food preparation and physical eating and drinking difficulties (in association with an occupational therapist)
- recommending prescribed nutritional supplements
- discussing gastrostomy.
Eating and drinking
When someone has swallowing problems and can take in less food, the nutritional content of meals is particularly important. A dietitian can recommend a diet based on the assessment by a speech and language therapist. They will suggest different types of food and ways to fortify food to improve the nutritional content. They may recommend food supplements which are available on prescription.
Our Eating and drinking guide for people with MND includes information on how people can adapt how they eat and drink, if needed. It includes information, tips and easy-swallow recipes.
When eating and drinking become difficult, the following suggestions may help. However, it is best to seek advice from an speech and language therapist, as everyone’s swallowing ability is different.
Eating
- Choose softer food which is easier to chew.
- Cut the food finely on the plate or mash it well with a fork so it requires less effort to chew.
- Add extra sauce or gravy, as moist food is easier to swallow.
- As mealtimes become more difficult, people with dysphagia usually find that blended or puréed food is easier to swallow. It is often preferable to blend the different foods separately to retain the flavours, rather than blending the entire meal together.
In general, when someone has a swallowing problem, they should avoid:
- mixed textured foods and liquid with ‘bits’, eg minestrone soup
- foods that need a lot of chewing, eg fresh bread or some meats
- stringy food, eg celery or some green beans
- coarse, hard food, eg well done toast, or crumbly, dry food, eg biscuits or flaky pastry
- some vegetable skins which can be difficult to clear in the mouth, eg tomato or sweetcorn
- foods that become sticky in the mouth, eg bread or mashed potato.
Drinking
People with MND sometimes cough when drinking. This may be due to weakness and lack of co-ordination of the muscles used to swallow. It may be a sign of aspiration (drink going down towards the lungs). Thicker drinks tend to move more slowly and are therefore less likely to cause aspiration. An SLT might recommend a thickening powder, available on prescription, which can be added to drinks.
If drinking is difficult, an individual may gradually reduce their fluid intake. Choosing moist foods with a high fluid content, eg soups, casseroles, stewed fruit, ice cream and custard, helps to prevent dehydration and associated symptoms.
Gastrostomy
As swallowing problems progress, alternative feeding methods should be discussed with the person with MND. Exploring pros and cons will enable the individual to make an informed choice.
The following may be used to ‘top-up’ oral intake, to meet full nutritional and dehydration needs and to administer medications:
- Nasogastric tubes (NGT)
- Percutaneous Endoscopic Gastrostomy (PEG)
- Radiologically Inserted Gastrostomy (RIG)
- Per-oral Image-guided Gastrostomy (PIG).
With RIG, the feeding tube is inserted under x-ray guidance. PIG is a hybrid of PEG and RIG but at present is not widely available.
A nasogastric tube can be used in the short-term to build up someone who is malnourished or dehydrated, and who wants to proceed with gastrostomy, or it may be used for a longer period. This method may be used in people for whom other types of gastrostomy are not appropriate, or may be preferred by some. It is often considered less comfortable than gastrostomy tube placement.
PEG is the preferred method of gastrostomy when someone has good respiratory function, or PIG/RIG when there is significant compromise of respiratory function.
The optimal timing of gastrostomy is likely to be when someone has lost around 5% of their body weight (from measurement taken at diagnosis). Earlier placement of a gastrostomy tube is recommended, even if it isn’t used straight away, as when needed, it can improve/maintain quality of life.
Someone considering a gastrostomy needs to be aware of the level of support needed to manage living with this intervention. For example, who will manage the feeds in the community. If it is a family member, this person will need to understand what is involved and how often feeds should be administered, to ensure they can physically manage. If care support is needed, arrangements need to be made at an early stage.
Not everyone with MND will choose this type of intervention and their decision should be respected. Gastrostomy may be included in an Advance Decision to Refuse Treatment (ADRT).
Tools to support gastrostomy decision making
MyTube
Developed by Sheffield Institute for Translational Neuroscience (SITraN), MyTube is a useful online resource containing short videos and information about gastrostomy to help people with MND learn more about the intervention. It features both health professionals, and people with MND discussing their experiences.
Gastrostomy tube - is it for me?
Researchers at Southampton University have developed Gastrostomy tube - is it for me?, a web-based patient decision aid for people with MND considering a gastrostomy tube. It aims to help people living with MND choose whether they want to have a gastrostomy tube fitted now. If they decide not to go ahead, they may want to revisit the decision later.
If you would like to see the questions before recommending the tool to your patients, a PDF version of the tool is also available. The tool is the result of the DiaMoND research project led by Southampton University, funded by the MND Association and Marie Curie. The team who developed the tool have produced the short video below. You may wish to share this with your patients.

Constipation
Sphincter muscles are not normally affected by MND. Changes in bowel function are usually the result of:
- forced inactivity
- reduced peristalsis
- low fluid intake
- reduced fibre intake
- weakness of pelvic floor and abdominal muscles
- use of analgesics.
Treatment
- Maintain hydration and assess fibre intake.
- Use of softeners and stimulants may help. Liquid versions are available that can be given via a feeding tube.
- Use of suppositories, enemas or manual evacuation may be necessary on occasions.
- Remedies such as bulking agents and fruits with a high sorbitol content (eg prunes) are also readily available.
Diarrhoea may be due to constipation with overflow.
Saliva problems
Types of saliva problems
The salivary glands produce two different types of secretions: thin, watery saliva and thick mucus.Phlegm is a thick mucus secreted by the membranes of the respiratory passages. Someone with MND may experience thin, runny saliva that drools out of the mouth, thick tenacious saliva or phlegm. Thick saliva and phlegm can be difficult to clear.Some people may experience all of these.
Thin, watery saliva
People with MND may find they experience pooling of large amounts of thin watery saliva, which can cause drooling. Although a normal amount of saliva is produced by those with MND, around two to three pints every day, excessive saliva (sialorrhea) is a commonly reported symptom.In most cases, saliva problems are the result of poor saliva control, caused by poor lip seal and/or dysphagia. People who have MND may have weak muscles around the mouth, tongue and throat. This can make it more difficult to manage saliva, both in the mouth and during swallowing.
Thick, tenacious saliva, mucus and phlegm
Others complain more of thickened mucus in the mouth and throat, which is difficult to swallow, or phlegm in the airways, which is difficult to cough up due to weakened respiratory muscles and an ineffective cough.Thick mucus can build up in the mouth and at the back of the throat of someone with MND due to dehydration, mouth breathing or open mouth posture, which can lead to evaporation of saliva.This may produce stringy mucus and cause airways to become blocked. This can be very distressing for the person with MND and those who care for them.
Dry mouth
Some people will experience a dry mouth, which may be caused by the medication they are taking, thrush, a coated tongue, insufficient fluids or breathing through the mouth.
Role of professionals
The consultant or specialist nurse will usually manage saliva problems, either with:
- self-help techniques
- prescriptions
- organising equipment/treatment.
- This may vary where the specialist centre is not within easy reach. A speech and language therapist or physiotherapist may be able to provide suggestions or strategies to help with saliva control.
A speech and language therapist can:
- help to identify any problems that may be present. These may include poor lip seal and/or weakness in oral and facial muscles or the tongue. All of these can contribute to problems with saliva management
- give advice on different swallowing techniques that may make swallowing easier.
A physiotherapist can give advice on:
- cough management techniques, which may help to cough up thick, tenacious saliva.
- postural problems and ways to alter the person’s position. In some cases, improving posture may help to control the flow of saliva.
Neck weakness and a drooping posture can cause the head to tilt forward, and saliva may flow through the lips before it can be swallowed head supports or neck collars, which may improve the posture of the person with MND.
Medication
Medication should always be prescribed by a doctor or a professional trained as a prescriber.
Before medication is prescribed by an appropriate professional, the problem should be properly assessed. This is because medications that can ‘dry up’ or reduce watery saliva may lead to thick, tenacious saliva or can worsen the situation if saliva is already thick.
Other medicines, including those available without a prescription, should never be taken without consulting a doctor, as there may be contraindications.
Some people with MND will have an enteral feeding tube. Medication can sometimes be given through the tube, but before putting any medication through, check with a pharmacist that it won’t harden or clog the tube, or affect how well the drug works.
Management of sialorrhoea
The following medication recommendations are from the NICE guideline on MND. For dosages please refer to British National Formulary (BNF).
- Consider a trial of antimuscarinic medicine as the first-line treatment, eg hyoscine (tablets or transdermal patches – be aware of the possible side effect of causing confusion in the elderly) glycopyrronium bromide (glycopyrrolate).
- Consider glycopyrrolate as the first-line treatment for sialorrhoea in people with MND who have cognitive impairment, because it has fewer central nervous system side effects.
- If first-line treatment for sialorrhoea is not effective, not tolerated or is contraindicated, consider referral to a specialist service for Botulinum toxin A. Be aware that treatment with Botulinum Toxin A may have the side effect of increasing dysphagia, so some suggest only resorting to botulinum toxin injections if the person already has enteral feeding in situ. Botulinum toxin should only be administered by specialist practitioners.
Radiotherapy
Another possible treatment for excessive, watery saliva is the use of radiotherapy to destroy part of the salivary glands.
Suction
Portable oral suction units are helpful if saliva builds up in the mouth.
Management of thick, tenacious saliva
- Review all current medicines, especially any treatments for sialorrhoea.
- Provide advice on swallowing, diet, posture, positioning, suctioning, hydration and pay attention to oral hygiene – consult district nurse.
- Consider treatment with humidification, nebulisers and carbocisteine. Carbocisteine is available as capsules or liquid, which can be administered via a feeding tube.
Treatments and strategies for dry mouth
- Dosage of medication should be checked by a prescribing professional and changed if needed.
- Preparations such as artificial saliva sprays or gels, for example Aquoral, Biotene Oralbalance or Xerotin, can help to relieve a dry mouth. They also help to reduce odour-causing bacteria. These treatments are given using a swab around the mouth before meals or at bedtime. Some of these items are available without a prescription.
- Oral hygiene should also be checked. A district nurse may be able to help with this. The teeth, tongue and gum margins should be cleaned regularly and especially before oral medication is given.
- The amount of fluid taken in by the person with MND should be increased, whether orally or through a feeding tube. A dietitian can advise on ways to increase fluid intake.
- Some people have found that, particularly at night, rapeseed or groundnut oil (where appropriate) or ghee can be used as a lubricant when swabbed around the mouth.
Page last updated: July 2023
Next review: July 2025